Procrustes took in lodgers on the road to Athens, but they had to fit his proffered bed. If the prospective lodgers were too short, he stretched them, and if they were too tall, he cut as many inches as necessary from their legs. As a result, according to Encyclopedia Brittanica, “The ‘bed of Procrustes,’ or ‘Procrustean bed,’ has become proverbial for arbitrarily—and perhaps ruthlessly—forcing someone or something to fit into an unnatural scheme or pattern.”
Enter American Obstetrics.
Human beings generally are within a range of normalcy. As such, we do not expect everyone to be exactly the same height or weight. We don’t say that everyone should have exactly the same blood sugar reading, and we accept a range of blood pressure readings as healthy. A woman could be 5 feet or 6 feet tall–we might think that one woman was short and the other tall, but we probably wouldn’t consider either to be abnormal–certainly not to the point that we would medically intervene to change her. There is an average, to be sure, but there is a range around that average that is considered “normal.”
But that range, in the mind of an obstetrician, may become very, very small.
A friend of mine, pregnant with twins, had one twin who was substantially smaller than the other. As the pregnancy came close to 36 weeks gestation, the OB ran some tests to see if the smaller twin was suffering from intrauterine growth restriction. The numbers came back within the normal range, but the doctor didn’t like them because they were on the low side of normal. She told my friend that a cesarean was necessary, and as a result, the larger twin, not ready to be born, spent a week in the NICU with respiratory problems.
The length of a normal, healthy pregnancy can vary by as much as 5 weeks, but new definitions recommended by the American College of Obstetricians and Gynecologists (ACOG) have narrowed the definition of normal gestation to a 2 week window. Only babies born at 39-41 weeks are “term”:
Recommended Classification of Deliveries From 37 Weeks of Gestation
As Linda Hunter observes, accurately calculating a due date from the first day of the last menstrual period (LMP) depends on “the woman’s accurate recall of her LMP; the regularity of her cycles; the presence of early or light bleeding; and other factors, such as oral contraceptive use or breastfeeding that could influence ovulation timing. There can also be some variation in the actual timing of ovulation, even in the presence of a seemingly normal 28-day menstrual cycle.” And many women do not have 28 day cycles, though the due date is generally calculated the same way regardless.
Ultrasound screening is generally more accurate at estimating gestational age than using the LMP, but this method also has limits. Hunter reminds us that screening is only reliably accurate if done in the first trimester. In addition, she says, “Ultrasound’s accuracy depends greatly on the skill of the person performing the examination and the quality of the images, not to mention the size of the patient and the fetal position.” She notes that ultrasound dating is useful because many women’s due dates are estimated too early under the LMP method, and thus many women undergo unnecessary inductions for “postdate” pregnancies (late term or post term, according to the new definitions) that are actually still well within the “term” range.
Even within the two week window, many OBs push for induction as soon as a woman reaches 39 weeks. The average pregnancy length has become shorter and the range of gestational age at birth narrower as induction has more frequently been used to force women’s bodies to conform to obstetrical definitions of term. In the past decade, the average length of pregnancy has decreased from 40 to 39 weeks, in part because of scheduled inductions and cesareans to make women’s pregnancies fit an increasingly narrow definition of “normal.”
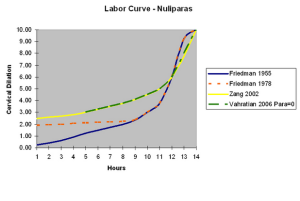
Perhaps the most egregious narrowing of the normal window comes from Friedman’s curve. Friedman observed the labors of women in the 1950s, and came up with a”normal” trajectory for a labor to progress (click to enlarge):
As Rebecca Dekker at Evidence Based Birth explains, Friedman’s curve is now obsolete. Women are no longer heavily sedated in labor. Their size is different, their nutrition is different, their lifestyles are different, and most women labor much longer now than they did during the time of Friedman’s observations. Here is a graph that shows Friedman’s curve against the typical labors of contemporary women (click to enlarge):
Despite the historical changes, many OBs cling to Friedman’s curve as the definition of “normal” labor, and give women Pitocin and other drugs to try to make an uncomplicated labor conform to Friedman’s curve. If the woman’s body still does not conform, she may wind up with a cesarean for “failure to progress,” even though her labor was progressing fine.
A debate has now arisen over diagnosis of gestational diabetes (and I’m sure this debate will continue). New standards proposed would lead to nearly 20% of pregnant women being diagnosed with gestational diabetes. Although the NIH issued a consensus statement that the old standards should remain for now, some doctors are now concerned by blood sugar readings that were considered perfectly normal by everyone just a few years ago. It should be noted that women experience many negative effects with a diagnosis of gestational diabetes, including “constant worry and anxiety over their baby, self-blame and guilt, and more medicalization throughout the prenatal care and delivery,” all of which, like gestational diabetes itself, can lead to negative health consequences.
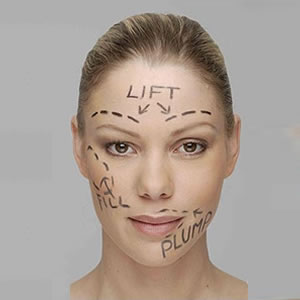
The narrowing range of obstetric normalcy mirrors other areas in which women are expected to conform to a narrow standard–and literally to cut their bodies to conform:
There are many ways to be a human being and to grow one. In the words of Dr. Anne Marie Jukic,
[N]atural variability may be greater than we have previously thought, and if that is true, clinicians may want to keep that in mind when trying to decide whether to intervene on a pregnancy.
Women do not need to be cut open because their bodies do not follow a line on a graph. They do not need to be shamed and blamed for numbers a doctor doesn’t like. They do not need to be given medications to force their functions to fit a preconceived idea of what is normal. Perhaps instead someone could observe the woman and her fetus and see if both appeared to be healthy and developing well, and intervene only when an actual problem arose.
Fitting into a Procrustean version of obstetrics that dictates increasingly narrow ranges of normal does not benefit women or babies–and rejecting such a model would allow more women to emerge from pregnancy and birth physically and psychologically intact.