New recommendations from both the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal Fetal Medicine (SMFM) seem revolutionary. Their new joint consensus statement advises abandoning the time restrictions on labor established by misguided adherence to Friedman’s Curve. Here are some of the new recommendations, which are designed to lower the primary cesarean rate:
- Allowing prolonged latent (early) phase labor.
- Considering cervical dilation of 6 cm (instead of 4 cm) as the start of active phase labor.
- Allowing more time for labor to progress in the active phase.
- Allowing women to push for at least two hours if they have delivered before, three hours if it’s their first delivery, and even longer in some situations, for example, with an epidural.
- Using techniques to assist with vaginal delivery, which is the preferred method when possible. This may include the use of forceps, for example.
Aside from being written as if an epidural is unusual (60%-80% of first time mothers have epidurals), these guidelines have amazing potential to lower the rate of cesareans by justifying longer time for women to labor and reducing obstetricians’ justifications for their “failure to wait.”
The question remains, however, whether these new guidelines really will change practice in any meaningful way. Even the joint consensus statement from ACOG and SMFM says,
Changing the local culture and attitudes of obstetric care providers regarding the issues involved in cesarean delivery reduction also will be challenging.
They go on to note that systemic change (meaning things like changes in required hospital protocols) is likely to be essential for significant practice change to occur, and they also argue for tort reform (discussed below).
People often say that obstetricians perform cesareans because the reimbursement is higher, and there are studies that indicate that this is true. Doctors, however, are not always paid more for cesareans, and when they are, the difference is often only a few hundred dollars–not chump change, but probably not the major motivator for those in one of the most highly paid medical specialties. The increase in birth costs for cesareans is primarily for the hospital resources: the operating room, post-operative care, and a longer hospital stay for the woman and her baby. Contrary to what some studies have found, according to a conversation I had with Alabama Medicaid officials, when Alabama changed its Medicaid reimbursement a few years ago to be the same for cesareans and vaginal births, officials were disappointed to find it did not reduce the cesarean rate. Here is a graph based on CDC data from Jill Arnold’s CesareanRates.com:
So what does drive high cesarean rates if it’s not all about the financial greed of physicians looking to make a couple hundred bucks through slice and dice obstetrics?
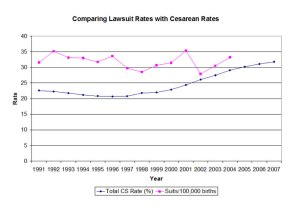
Some cite malpractice suits as a major motivator. While malpractice premiums do appear to impact c-section rates, the effect is relatively small. Rather than actual malpractice suits, according to Theresa Morris’ Cut it Out, it is fear of them that drives OBs toward cesareans. According to Childbirth Connection’s comprehensive report, Maternity Care and Libility, ACOG’s 2009 survey of OB practitioners reported that liability fears had led 29% of respondents to increase their use of cesarean and 26% to stop performing VBACs. Here’s another graph from Jill:
In his excellent New Yorker article on “how childbirth went industrial,” Atul Gawande points to the predictability and reliability of cesarean over vaginal birth, which makes doctors likely to choose cesarean over less invasive procedures (such as forceps deliveries) that may be risky in the hands of those without enough training, experience, or practice:
Is medicine a craft or an industry? If medicine is a craft, then you focus on teaching obstetricians to acquire a set of artisanal skills….if medicine is an industry, responsible for the safest possible delivery of millions of babies each year, then the focus shifts. You seek reliability. You begin to wonder whether forty-two thousand obstetricians in the U.S. could really master all these techniques….[O]bstetricians decided that they needed a simpler, more predictable way to intervene when a laboring mother ran into trouble. They found it in the Cesarean section….We have reached the point that, when there’s any question of delivery risk, the Cesarean is what clinicians turn to—it’s simply the most reliable option….Clinicians are increasingly reluctant to take a risk, however small, with natural childbirth.
Yet c-sections also pose real risks, as this table from the joint consensus statement indicates:
(Note that cesarean’s near-quadrupling of maternal death risk is not causing a call to ban non-medically essential cesarean).
Another factor in physician preference for cesarean–one that is closely tied with money–is time. As one prominent obstetrician once told me, the money itself isn’t the issue–what’s a couple hundred dollars to someone whose salary is well into six figures? It’s time. A cesarean takes 40 minutes. A vaginal birth can drag on for hours and hours, and the timing is completely unpredictable.
This report on Maternity Care Payment Reform from the National Governors Association explains that the optimum timing possible with cesarean is personally convenient as well as financially lucrative–but not because of the payment for the cesarean itself:
[P]lanned cesarean deliveries have lower opportunity costs for obstetricians and facilities. For facilities, spontaneous vaginal deliveries may be more difficult to plan and manage compared to scheduled cesarean deliveries. With a planned cesarean delivery, hospitals can schedule operating room time and ideal hours for nursing staff. For providers, scheduling a cesarean birth ensures that they will be the ones to perform the delivery and they will not have to transfer care and associated payment to a colleague or be delayed from office or other hospital duties.11 In addition to securing reimbursement, having scheduled births allows providers more time to schedule billable procedures.
Even in vaginal births, the emphasis many obstetricians put on time is obvious. Elective inductions allow for births to be scheduled at the physician’s convenience (and while this may sometimes be convenient for the pregnant woman also, you can bet that she does not get to pick a time that would be inconvenient for her doctor). ACOG guidelines on labor induction and augmentation discuss the reduction in labor time that can occur with Pitocin administration in positive terms (without any indication that this is preferred by laboring women).
In my tours of hospital labor units, it has not been uncommon for every laboring woman on the board to have a Pitocin drip to “help them along.” A friend of mine–one who was amenable to a highly medicalized birth and had an epidural in place–said her obstetrician walked into the room when she had dilated to 10 centimeters and said, “Okay, you have two hours to push this baby out and then I’m going to have to do a cesarean.” This did not even meet old time guidelines, which indicated a three hour pushing time for first time mothers who had an epidural.
The website My OB Said What? is full of anecdotes about practitioners who value their own time over the normal progression of labor. A few examples:
- “Well she pushed for over two hours, I would have just sectioned her.”– OB who was not caring for the mother during labor, after learning of the mother’s vaginal birth.
- “But then we’ll be here ALL DAY!” – OB, with wild flinging of arms into the air, in response to the suggestion that breaking the bag of water be delayed until a mother being induced continued to dilate more then the current 2 CM of dilation she was at.
- “You can’t pay me enough to sit here waiting for you to deliver to make up the time lost with my children.” –OB commenting on Twitter.
- “You’ll have to be pushing by 1, I have some place to be at 2 this afternoon.” –OB to woman on Pitocin induction who was also having her membranes ruptured at 2cm dilation.
Some doctors also feel a therapeutic mandate to “do something,” which is often counterproductive in a normal labor. Obstetrician and ethicist Paul Burcher notes that a “therapeutic imperative” is essentially another term for “the inertia that prevents physicians from abandoning ineffective therapies because no better alternative yet exists.” Burcher is writing about bed rest, but as with threatened miscarriage, the current “better alternative” in a normal labor is to do nothing at all. As Dr. Burcher says,
It takes courage to do nothing, but when we have nothing of benefit to offer we must refrain from deluding ourselves and harming our patients.
Here’s hoping that ethics will trump time and money and lead to genuine change in practice. But given the historic difficulties obstetricians have with implementing evidence based practice and the slow obstetric response to reducing (rather than increasing) intervention, given the average time it takes to put an innovation into routine practice, we may have at least 17 years to wait.